Treatment & Management
Although there is no cure, there are more effective psoriasis treatments today than ever before. Treating psoriasis can help improve symptoms as well as lower the risk of developing psoriasis comorbidities such as psoriatic arthritis, heart disease, obesity, diabetes, and depression.
Treatments for psoriasis include:
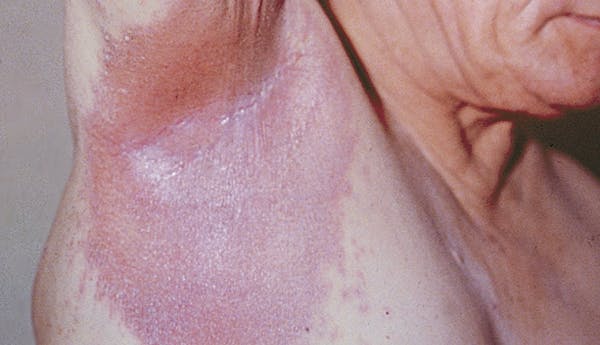
Because skin folds can be prone to yeast and fungal infections, your health care provider may prescribe a combination of treatments. Do not occlude (cover) skin folds unless directed by a health care provider. To keep the lesions in skin folds dry and to lower the risk of fungal infection, your provider may recommend the use of powders to dry the moist lesions.
Over-the-Counter Products
Over-the-counter (OTC) products may help manage symptoms if you have mild psoriasis. If you are looking for OTC products to try, check out NPF's Seal of Recognition program. These products have been created or are intended to be non-irritating and safe for people with psoriasis.
Prevention
There is no known way to prevent the onset of psoriasis, however, there are many ways that you can manage your triggers to reduce flares.
Outlook/Prognosis
Psoriatic disease is lifelong, and symptoms may resolve and recur throughout the lifetime.
While there is no cure for psoriasis, treatments today are more effective than ever before and research into new treatments, as well as a cure, is ongoing. Treating psoriasis can help improve symptoms and may decrease the associated inflammation that can lead to psoriasis comorbidities such as psoriatic arthritis, heart disease, and depression.